Recently a critical care specialist at one of The Resuscitation Group ACLS EP courses remarked that normal saline is the most dangerous drug in common use today, and it is most certainly not a physiological resuscitation fluid.
While we do believe there are issues of significant weight with saline use in healthcare, many are confused by the prevalence of use and financial concerns, or worse by their misunderstanding of the science.
Realistically, at this point in the science, a patient care provider should reconsider whether saline use can continue in their environment.
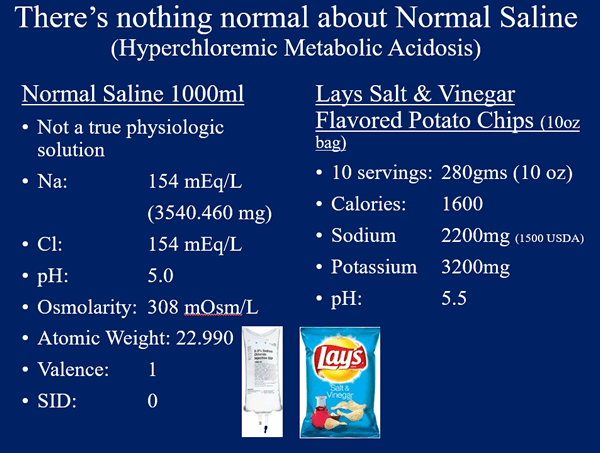
If you were, for bizarre reasons, forced to mix normal saline from sterile salt and sterile water; you would have to say that sodium chloride has a molar weight of 58.44 grams, and so 150mmol of it weighs 8.77 grams. This is more sodium and a lower pH than a bag of Lays Sea Salt and Vinegar Chips!
There is an excellent article detailing the history of saline solutions, co-authored by one of the experts in fluid physiology Dileep N. Lobo (Awad, Sherif, Simon P. Allison, and Dileep N. Lobo. "The history of 0.9% saline." Clinical nutrition 27.2 (2008): 179-188). We will not make an attempt to improve on a foundational coverage of the topic done in this article. Instead, we offer a brief, but inadequate, summary and explanation. Apparently, the whole concept of infusing electrolyte-laden water into patients arose during the great cholera epidemics of the 1830s. Learned authors of the day tried to published on the effects of resuscitation fluids which were composed of "two drachms of muriate, and two scruples of carbonate, of soda, to sixty ounces of water".
The term "normal saline" entered the popular medical vernacular after an 1888 Lancet paper lauded its effects in resuscitating a "prostrate and pulseless’’ patient. However, the content of the fluid used in that case (or most subsequent cases) was totally unlike the normal content of extracellular fluid. The first description of a 0.9% NaCl solution as "isotonic" had come from Hartog Jacob Hamburger, who performed freezing point experiments and observed hemolysis, concluding that 0.9% NaCl was isotonic with mammalian body fluids.
In the end, the only science in support of 0.9% saline in clinical practice was based solely on Hamburger’s in vitro study from the 1800’s.
So, let us go back to the students of today, indoctrinated by a healthcare system which has had little introspection into the things we do for resuscitation until the 1980’s and the standardization of the science review systems and the classification of efficacies of the 2000’s through ILCOR and other science bodies.
As Dr. Fergal Cummins, frequently says “people don’t know what they don’t know”. Initially, as we are sure you can imagine, this caused us much dissonance, but we have grown to realize that it sums up the state of our healthcare professions completely.
It is quite difficult to keep up on one’s specialty areas, let alone have time for current resuscitation science. It has also become sport to create doubt with studies and science, but in this case, while people have focused on the SMART and SALT-ED trails, they are not the only evidence that we have been on the wrong track. Nor is Normal Saline the only fluid under significant negative findings, Colloids and HES were found so negative to outcome the CRYSTMAS Study said that HES should no longer be used in the
critically ill patient and it should be stopped immediately.
Unlike the issue with many items in resuscitation; Normal Saline is a primary mortality cause, not a contribution to mortality.
Saline exacerbates acidosis; saline causes hyperchloremic acidosis. Some patients we resuscitate are severely acidemic to begin with; it is irresponsible to give them a fluid which will exacerbate their acidemia. If saline is used as the default resuscitative fluid, then it will be given to acidemic patients before their labs return. Healthcare systems should be designed to avoid causing harm. Using saline as a default fluid is a poor choice, because it will inevitably lead to a situation where a severely acidemic patient is given an acidic fluid, causing deterioration. This is a failing at the system level. The fix is to use a balanced crystalloid as the default resuscitative fluid. Balanced fluids will always pull the patient's pH towards normalcy, so they are safe regardless of the patient's electrolytes. For example, if LR is given to a patient with metabolic acidosis, it will tend to increase the patient's pH toward normal. Alternatively, if LR is given to a patient with metabolic alkalosis, it will tend to decrease the patient's pH towards normal. LR isn't always the ideal fluid to fix a patient's acid-base abnormality. However, LR will always be safe, with a tendency to pull the pH towards normal.
Traditional dogma is that Lactated Ringer’s is unsafe in hyperkalemia. This myth has been debunked multiple times; evidence suggests the exact opposite of traditional dogma! Saline may be dangerous in hyperkalemia. The reason for this is that saline causes acidosis, causing potassium to shift into the blood. Four RCTs performed during renal transplant surgery all showed that saline causes more frequent episodes of hyperkalemia when compared to either LR or Plasmalyte (O’Malley 2005, Khajavi 2008, Modi 2012, Weinberg 2017). It’s unclear how generalizable this is; from a physiologic standpoint, it ought to be universal. For example, Martini 2013 found similar results when comparing LR vs. NR in a pig model of hemorrhagic shock. However, patients with adequate renal function may be able to compensate for potassium entering the blood.
Saline may cause hemodynamic instability. Potura 2015 performed a RCT on patients undergoing renal transplantation randomized to receive saline vs. Elomel Isoton solution (an acetate-buffered balanced crystalloid). Patients receiving saline required vasopressors more frequently (30% vs. 15%, p=0.03). However, this was a secondary endpoint. Pfortmueller 2018 investigated this finding further with a double-blind RCT comparing normal saline vs. Elomel Isoton solution in patients undergoing major abdominal surgery. Patients receiving saline required vasopressors more frequently. Both groups of patients received about three liters of fluid, producing moderate differences in electrolyte levels; but this study is limited because it was halted early due to harm caused by saline!
Saline may lead to increased levels of inflammation. Kellum 2006 showed that in septic rats, using hydrochloric acid to induce a hyperchloremic acidosis increased levels of pro-inflammatory cytokines. Similarly, Zhou 2014 found that in a rat sepsis model, resuscitation with saline produced higher levels of interleukin-6, compared to resuscitation with Plasmalyte. Wu 2011 performed a RCT of patients with pancreatitis that included a comparison between LR and NS. Patients treated with NS had higher levels of C-reactive protein one day after the initiation of resuscitation. Normal saline also seemed to delay resolution of clinical features of systemic inflammation (SIRS criteria).
Saline causes kidney injury. Hyperchloremia causes renal vasoconstriction, so saline is expected to impair renal function. This was indeed found in a rat sepsis model, where saline resuscitation increased the rate of kidney injury compared to Plasmalyte (Zhou 2014). In normal human volunteers, a two-liter saline bolus reduced blood flow to the renal cortex, compared to two liters of Plasmalyte (Chowdhury 2012). Yunos 2012 performed a landmark before-after study, which involved a structured intervention to avoid chloride-rich resuscitative fluids in an ICU. Following this intervention, the rate of acute kidney injury decreased. Meta-analysis including this trial, small RCTs, and retrospective studies supported the concept that saline causes renal failure. The SALT-ED trial is a pragmatic cluster-randomized multiple-crossover study performed at the Vanderbilt emergency department. The default resuscitation fluid was alternated monthly between saline and balanced crystalloids (LR or Plasmalyte). This study involved patients being admitted to the hospital ward. A secondary endpoint was adverse kidney events: a composite of death, dialysis, or doubling of the creatinine within one month.
The study included 13,347 patients, who received a median of one liter of fluid. 95% of patients randomized to receive balanced crystalloid were treated with LR, so this was effectively a trial of saline vs. LR. Saline increased the risk of death or renal failure (5.6% vs. 4.7%, p=0.02), with the difference driven mostly by differences in renal failure. As might be expected, the subgroup of patients with renal injury at admission was more susceptible to harm from saline (37.6% vs. 28% adverse kidney events, p<0.001).
The SALT-ED trial confirms that saline increases the risk of renal failure. This trial is remarkable because saline was harmful even at a low dose, in stable patients. Due to the massive size of this study it was able to detect a small difference in renal failure, which would have been missed by most studies. In most situations, an effect size of 1% wouldn’t be impressive. However, switching from saline to LR is easy to do, at nearly no cost (~25 cents difference). The number needed to harm from saline is 111. This means that the cost of preventing one episode of renal failure is roughly $28. Given that an episode of acute kidney injury is estimated to cost $1700, switching from saline to LR would improve patient outcomes and save money (Silver 2017).
These are just some examples of multiple trails and studies on saline at this point.
Rather than any scientific rationale, the reasons for using saline boil down to the following:
- “It’s cheap.”
- “It’s what we have always done.”
- “Everyone in the department uses it.”
- “It's how I was trained.”
- “It seems to work.”
- “The nurses or the EPR select it automatically.”
This is a poor reflection on our healthcare profession if these are the reasons, we choose to do harm, and harm is what we are doing.
We are simply stating the science, and not unlike large volume ventilation from 20 years ago, some will continue to grasp for reasons to continue their current practice, but we at The Resuscitation Group cannot do that.
We wish to always fall on the side of advocating for change and preventing unnecessary harm to patients.